Research Article - (2022) Volume 10, Issue 1
Clinical teaching and learning during COVID-19 as perceived by nursing students in Lesotho: A descriptive cross-sectional survey
Isabel Nyangu1* and Libuseng Moureen Rathobei22Department of Nursing and Public Health, University of KwaZulu-Natal, Durban, South Africa
Received: 23-Mar-2022, Manuscript No. AERR-22-58243; Editor assigned: 28-Mar-2022, Pre QC No. AERR-22-58243 (PQ); Reviewed: 11-Apr-2022, QC No. AERR-22-58243; Revised: 18-Apr-2022, Manuscript No. AERR-22-58243 (R); Published: 28-Apr-2022, DOI: 10.51268/2736-1853-22.10.057
Abstract
Background: Nursing students and their clinical instructors in higher education institutions are faced with challenges regarding clinical teaching and learning strategies during the COVID-19 pandemic.
Objectives: This study aimed to determine the perceptions of nursing students regarding clinical teaching and learning during the COVID-19.
Methods: A descriptive quantitative survey was used to conveniently recruit 300 nursing students who were enrolled at selected higher education institutions in the 2021/22 academic year and they completed a structured self-report questionnaire. Permission to conduct the study was granted by relevant authorities (ID147-2021) and data were analyzed using SPSS (23).
Results: The minimum age of participants was 19 years and the maximum age was 39 years. The majority of respondents were female (69%: n=207) and studying for a BSc degree in Nursing and Midwifery (49%: n=146). Most nursing students had adequate knowledge, skills, and attitudes to prevent COVID-19 in the clinical area and simulation laboratories. They felt that clinical instructors and preceptors were available and competent to assist them in completing their clinical competencies and procedure file logbooks. Nursing students gained expertise in performing clinical procedures as they were able to perform return demonstrations in the simulation laboratory and clinical areas. Whilst clinical facilities and simulation laboratories had adequate COVID-19 prevention protocols and tools, there was inadequate personal protective equipment available.
Conclusion: The perceptions of nursing students regarding clinical teaching and learning during COVID-19 were positive. More support for adequate personal protective equipment for nursing students remains crucial for their training not to be interrupted.
Keywords
Clinical teaching, Learning, COVID-19.
Introduction
The COVID-19 pandemic brought significant interruption to nursing students’ education and training (De Ponti R et al., 2020). In response, clinical instructors around the world are scrambling to familiarize themselves in ways that facilitate the on-going knowledge, skills, and attitude development of the nursing students in the clinical placements while social distancing and other measures are distracting standard practices (Eva KW et al., 2020). Rose suggested that this pandemic presents practical and logistical challenges and concerns for patient safety in the hospital, knowing that nursing students may spread the virus when asymptomatic and may acquire the virus in the course of nursing training (Rose S, 2020). Therefore, this creates unprecedented clinical teaching and learning opportunities for nursing students in terms of exposure to special situations that encourage creativity and initiative (Newell EG, 2020; Matlala S, 2021).
According to Jamshidi et al., nursing education is composed of two complementary parts; theoretical training and practical training experiences that enable nursing students to acquire knowledge, skills, and attitudes for providing nursing care to patients (Jamshidi N et al., 2016). Therefore, nursing students’ competence is based on knowledge and skills taught to them by the clinical instructors (Manninen E, 1998). Consequently, a large part of nursing education is carried out in the clinical environments as nursing is a performance-based profession hence clinical learning environments play an important role in the acquisition of professional abilities and skills in caring for patients (Manninen E, 1998). Furthermore, Phillips et al. suggested that clinical learning environments provide nursing students with opportunities to practice and become proficient in the knowledge and skills essential for professional practice (Phillips KF et al., 2017). Additionally, Jamshidi et al. stated that clinical learning environment provides an opportunity for nursing students to learn experimentally and to convert theoretical knowledge to a variety of mental, psychological, and psychomotor skills which are crucial for the patient care (Manninen E, 1998).
The contagious nature of COVID-19 has prohibited nursing students from being active members of clinical teams as hospitals attempts to minimize non-essential staffing in clinical environments, which compromised their clinical teaching and learning (Dedeilia A et al., 2020; Matlala S, 2021). Conversely, Woolliscroft stated that despite the educational value and diversity of available online resources, lack of bedside training compromises students’ direct involvement with patients, which could have optimized their physical examination skills as well as several non-technical skills (Woolliscroft JO, 2020). Furthermore, Koumpouras and Helfgott added that patients’ clinical assessments are halted in virtual reality, preventing nursing students’ engagement with feedback through direct observation of clinical skills or supervised learning events by their nurse clinical instructor (Koumpouras F et al., 2020).
Problem statement
COVID-19 has relentlessly spread even in the least developed countries, severely disrupting the lives of people living in their dominions, which have not developed effective virtual reality or online platforms to effectively respond to the current challenges presented by the pandemic (Cecilio-Fernandes D et al., 2020). This brought nursing students’ clinical and theoretical education to be disproportionately affected as many institutions closed campuses (Dedeilia A et al., 2020). Woolliscroft stated that the shortage of coronavirus tests and personal protective equipment, as well as suspension of regular clinical care such as out-patient clinics or elective surgeries, has precluded students from being active members of clinical teams as hospitals attempt to minimize non-essential staffing in clinical environments (Woolliscroft JO, 2020). However, Farooqi et al. asserted that various education departments across the world took measures to advise the HEIs to transform all academic teaching online (Ansari KA, 2021). In addition, Woolliscroft reported that despite the educational value and diversity of available online resources, the lack of bedside nursing training compromises students’ direct involvement with patients which could optimize their physical examination skills (Cecilio-Fernandes D et al., 2020). Conversely, students perceived that the virtual environment was appealing, enjoyed using the virtual environment, and perceived that the virtual environment was fast (Botha BS et al., 2021).
Currently, there is no data or Evidence-Based Research (EBR) on the perceptions of nursing students and their clinical instructors regarding clinical teaching and learning strategies during COVID-19 in Lesotho. This study, therefore, sought to gain insight into perceptions of nursing students regarding clinical teaching and learning during COVID-19 at the selected HEIs in Lesotho.
Purpose of the study
The purpose of this study was to describe the perceptions of nursing students regarding clinical teaching and learning during COVID-19 at selected HEIs in Lesotho.
Materials and Methods
A descriptive quantitative survey was used to collect data from 300 nursing students who were enrolled at selected higher education institutions in the 2021/22 academic year in Lesotho. Convenience sampling was used to recruit the respondents who completed a structured self-report questionnaire. A pre-test of the data collection tool was conducted to ensure validity and reliability. Permission to conduct the study was granted by the National University of Lesotho (NUL) Institutional Research Board (IRB) and the Lesotho Ministry of Health Research and Ethics Committee for approval (ID147-2021). Written informed consent was given by the respondents who were identified using codes. All research data was encrypted and stored in a lockable cupboard. Virtues of sensitivity, respect, and patience were applied during contact periods with respondents. Respondents were asked to voluntarily take part in the study and could withdraw without any prejudice. Data were analyzed using the Statistical Package of Social Sciences (SPSS vs. 23) and presented using tables and graphs and described analytically.
Results
Demographic information
A total of 276 students out of 300 provided their age. The minimum age was 19 years and the maximum was 39 years (Range 20 years). The mean age was 23 years (± 3). Further illustrates the age of the respondents (Table 1).
| Age | N | Minimum | Maximum | Mean | Std. Deviation |
|---|---|---|---|---|---|
| 276 | 19 | 39 | 23.04 | 3.269 |
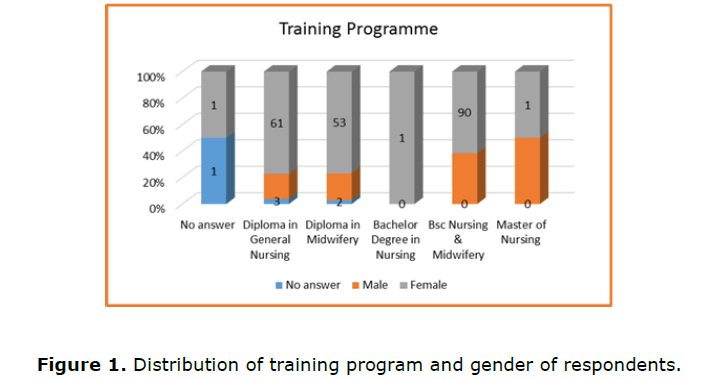
Males constituted 29% (n=86), females were 69% (n=207), less than 1%(n=1) selected other, whilst 2% (n=6) did not provide an answer. Majority (80%; n=240) of the nursing students were single, 9% (n=26) were married, 1% (n=4) were engaged, 2% (n=6) were cohabiting, 7% (n=21) preferred not to say, whilst 1%(n=3) did not answer. The majority, (93%; n=279) were Christian, 2% (n=5) were African Traditionalists, 1% (n=3) were either Muslim, selected other, or did not provide an answer, whilst less than 1% (n=1) were Hindu.
Sampling and population
The majority (49%; n=146) of the nursing students were studying for a BSc degree in Nursing and Midwifery, 0.3% were studying for a Bachelor degree in Nursing, 26% (n=79) were studying for a Diploma in General Nursing, 23% (n=70) were studying for a Diploma in Midwifery, whilst 0.7% (n=2) were studying for a Master degree in Nursing. Further illustrates the distribution of the training programme and gender (Figure 1).
The population was calculated using the sampling calculators (Government of the Republic of Malawi, 2013; Taherdoost H, 2016). The respondents comprised academic staff, students (Bachelors, Masters, and Ph.D.), academic institution leadership (Deans and head of departments).
Nursing student’s perceptions on clinical teaching and learning during COVID-19
When asked if they had adequate knowledge on COVID-19, majority (54%; n=163) of the students agreed, 29%:(n=87) strongly agreed, 11% (n=33) were not sure, 3% (n=9) disagreed, 2% (n=5) strongly disagreed, whilst 1%(n=3) did not answer. The perceptions on adequate knowledge on COVID-19 were not associated with the training programme [X2 (25, N=300)=27.45, p>0.05].
When asked if they had adequate skills and knowledge to prevent COVID-19 in the simulation laboratory, a majority (51%; 153) of the students agreed, 27% (n=81) strongly agreed, 15% (n=45) were not sure, 5% (n=14) strongly disagreed, 2% (n=6) disagreed, whilst less than 1% (n=1) did not answer. The perceptions on adequate skills and knowledge were associated with the training programme [X2 (30, N=300)=52.56, p<0.05].
When asked if they had adequate skills and attitudes to prevent COVID-19 in the clinical area, a majority (53% (n=153)) of the students agreed, 26% (n=77) strongly agreed, 14% (n=40) were not sure, 4% (n=13) strongly disagreed, 3% (n=10) disagreed, whilst less than 1% (n=1) did not answer. The perceptions on skills and attitudes to prevent COVID-19 in the clinical area were associated with the training programme [X2 (25, N=300)=55.6, p<0.05].
Multiple When asked if there was adequate personal protective equipment in the simulation laboratory, a majority (33%; n=99) of the students disagreed, 23% (n=67) strongly disagreed, 21% (n=64) were not sure, 19% (n=58) agreed, whilst 4% (n=12) strongly agreed. Perceptions on adequate PPE in simulation laboratory were associated with the training programme [X2 (20, N=300)=51.87, p<0.05].
When asked if there was adequate personal protective equipment in the clinical area, a majority 24% (n=71) of the students strongly disagreed, 24% (n=71) disagreed, 31% (n=92) agreed, 12%(n=37) strongly agreed, 9% (n=28) were not sure, whilst less than 1% (n=1) did not answer. Perceptions on adequate PPE in the clinical area were associated with the training programme [X2 (25,N=300)=72.69, p<0.05].
The When asked if clinical instructors were available at the simulation laboratory, a majority (49%; n=145) of the students agreed, 22% (n=67) strongly agreed, 10% (n=30) were not sure, 8% (n=23) strongly disagreed, 8% (n=25) disagreed, whilst 3% (n=10) did not answer. Perceptions on availability of clinical instructors in the simulation laboratory were associated with the training programme [X2 (25,N=300)=70.4, p<0.05].
When asked if clinical instructors were available at the clinical area, a majority (41%; n=145) of the students agreed, 12% (n=35) strongly agreed, 23% (n=69) disagreed, 16% (n=48) strongly disagreed, 6% (n=18) were not sure, whilst 2% (n=5) did not answer. Perceptions on availability of clinical instructors in the clinical area were associated with the training programme [X2 (25,N=300)=41.61, p<0.05].
When asked if preceptors were available in the clinical area, a majority (41% (n=123) of the students agreed, 10% (n=29) strongly agreed, 24% (n=71) were not sure, 12%(n=38) disagreed, 9% (n=28) strongly disagreed, 4% (n=11) did not answer. Perceptions on availability of preceptors in the clinical area were not associated with the training programme [X2 (25,N=300)=22.38, p>0.05].
When asked if they were able to perform return demonstration in the simulation laboratory, majority, (40%; n=149) of the students agreed, 26% (n=77) strongly agreed, 10% (n=30) disagreed, 6% (n=18) strongly disagreed, 6%(n=18) were not sure, whilst 3% (n=9) did not answer. Perceptions whether return demonstrations were performed in the simulation laboratory were not associated with the training programme [X2 (35,N=300)=38.37, p>0.05].
When asked if they were able to perform return demonstrations in the clinical area, majority (48%; n=143) of the students agreed, 29% (n=88) strongly agreed, 10% (n=30) disagreed, 4% (n=12) strongly disagreed, 7% (n=21) were not sure, whilst 2%(n=6) did not answer. Perceptions on whether return demonstrations were performed in the clinical area were not associated with the training programme [X2 (25, N=300)=31.6, p>0.05].
When asked if they were able to complete all the required clinical competencies in the previous academic year, majority, (30%; n=91) of the students agreed, 16% (n=47) strongly agreed, 24% (n=71) disagreed, 14% (n=43) strongly disagreed, 15%(n=44) were not sure, whilst 1% (n=4) did not answer. Perceptions on whether they completed all clinical competencies in the previous academic year were associated with the training programme [X2 (30, N=300)=52.35, p<0.05].
When asked if there were adequate COVID-19 prevention protocols at the clinical facility, majority, (48%; (n=145)) of the students agreed, 15% (n=45) strongly agreed, 18% (n=53) disagreed, 4% (n=13) strongly disagreed, 13% (n=38) were not sure, whilst 2% (n=6) did not answer. Perceptions on the adequacy of COVID-19 prevention protocols were associated with the training programme [X2 (25, N=300)=39.8, p<0.05].
When asked if clinical teaching during COVID-19 allowed them to gain expertise in performing clinical procedures, majority, (38% (n=115)) of the students agreed, 10% (n=30) strongly agreed, 21% (n=63) disagreed, 16% (n=48) strongly disagreed, 14% (n=42) were not sure, whilst 1% (n=3) did not answer. Perceptions on whether clinical teaching allowed them to gain expertise in performing clinical procedures were associated with the training programme [X2 (40,N=300)=55.79, p=0.05].
When asked if their procedure file log books were completed and submitted, a majority (32%; n=96) of the students agreed, 11% (n=32) strongly agreed, 31% (n=93) disagreed, 11% (n=35) strongly disagreed, 14% (n=41) were not sure, whilst 1% (n=3) did not answer. Perceptions on whether their procedure files were completed and submitted were associated with the training programme [X2 (25, N=300)=84.75, p<0.05].
When asked if they felt they had received adequate skills through clinical skills training, the majority (38%; n=112) of the students agreed, 6% (n=19) strongly agreed, 29% (n=88) disagreed, 13% (n=39) strongly disagreed, 13% (n=39) were not sure, whilst 1% (n=3) did not answer. Perceptions on whether they had received adequate skills training were not associated with the training programme [X2 (35,N=300)=34.14, p>0.05].
When asked if they felt their clinical supervisors were competent during the pandemic, majority (49%; n=148) of the students agreed, 7% (n=20) strongly agreed, 16% (n=48) disagreed, 9% (n=26) strongly disagreed, 18%(n=55) were not sure, whilst 1% (n=3) did not answer. Perception on whether clinical supervisors were competent during the pandemic were not associated with the training programme [X2 (30, N=300)=40.2 ,p>0.05].
The When asked if there were adequate patients during clinical practice, majority (38% (n=115)) of the students agreed, 32% (n=95) strongly agreed, 14% (n=42) disagreed, 7% (n=21) strongly disagreed, 6%(n=18) were not sure, whilst 3% (n=9) did not answer. Perceptions on the adequacy of patients during clinical practice were associated with the training programme [X2 (35, N=300)=58.1, p<0.05]. Further illustrates the perceptions of nursing students (Table 2).
| Perceptions | % response | |||||
|---|---|---|---|---|---|---|
| Strongly agree | Agree | Not sure | Disagree | Strongly disagree | No answer | |
| Adequate knowledge on Covid-19 | 29 | 54 | 11 | 3 | 2 | 1 |
| Adequate skills & knowledge to prevent Covid-19 in Simulation laboratory | 27 | 51 | 15 | 2 | 5 | 1 |
| Adequate skills & attitudes to prevent Covid-19 in clinical area | 26 | 53 | 14 | 3 | 4 | 1 |
| Adequate personal protective clothing in simulation laboratory | 4 | 19 | 21 | 33 | 23 | |
| Adequate personal protective clothing in clinical area | 12 | 31 | 9 | 24 | 24 | 1 |
| Clinical instructors available at simulation laboratory | 22 | 49 | 10 | 3 | 8 | 3 |
| Clinical instructors available at clinical area | 12 | 41 | 6 | 23 | 16 | 2 |
| Preceptors available at clinical area | 10 | 41 | 24 | 12 | 9 | 4 |
| Performed return demonstrations in simulation laboratory | 26 | 40 | 6 | 10 | 6 | 3 |
| Performed return demonstrations in clinical area | 29 | 48 | 7 | 10 | 4 | 2 |
| Completed all required competencies in previous academic year | 16 | 30 | 15 | 24 | 14 | 1 |
| There were Covid-19 prevention protocols at clinical facility | 15 | 48 | 13 | 18 | 4 | 2 |
| Clinical teaching allowed gaining of expertise to perform clinical procedures | 10 | 38 | 14 | 21 | 16 | 1 |
| Procedure file logbooks completed & submitted | 11 | 32 | 14 | 31 | 11 | 1 |
| Received adequate skills through clinical skills training | 6 | 38 | 13 | 29 | 13 | 1 |
| Clinical supervisors competent during pandemic | 7 | 49 | 18 | 16 | 9 | 1 |
| Adequate number of patients during clinical practice | 32 | 38 | 6 | 14 | 7 | 3 |
Discussion
The findings of the current study show that the minimum age of participants was 19 years and the maximum age was 39 years. This is in line with the study conducted by Michel et al. who reported that the majority (78.8%) of respondents in their study were aged 18 to 23 years (Michel A et al., 2020). The majority of respondents in this study were female, a finding congruent with Farooq et al. who stated that nursing students and nursing faculty are predominantly female in the situation of cultural context (Farooq F et al., 2020). Other studies also reported that the majority of the respondents were female (Mukhtar K et al., 2020; Michel A et al., 2020).
Respondents had positive perceptions as they felt they had adequate knowledge of COVID-19. This is in line with Albaqawi et al. who reported that nursing students had a good level of knowledge on COVID-19 and this knowledge was gathered from their government, Ministry of Education, and Social media (Albaqawi HM et al., 2020). Similarly, Asaad et al. stated that students reported that MERS-COV is a fatal disease and that healthcare professionals were at high risk of infection (Asaad A et al., 2020). However, Lovrić et al. revealed that students described the spread of misinformation on social networks and risky behaviours of the population (Lovric R et al., 2020). It, therefore, remains crucial to provide the students with trusted sources of information on the COVID-19 to prevent distortion.
Whilst respondents perceived that there were adequate COVID-19 prevention protocols in the clinical facility, they felt that there was inadequate personal protective equipment in the clinical areas. This is in line with Choi and Kim who reported that several respondents reported occasional problems with lack of protective masks and medical gloves for nursing interns in the hospital (Choi JS et al., 2016). Respondents had negative perceptions regarding the adequacy of PPE in the simulation laboratory. This is congruent with Ulenaers et al. who indicated that nursing students had experienced shortages of PPE in several clinical sites (Ulenaers D et al., 2021).
The majority of respondents had positive perceptions of their skills and knowledge to prevent COVID-19 in the simulation laboratory.
This is in line with Lovrić et al. who reiterated that students believed that transmission of disease (COVID-19) could be prevented following university precautions given by WHO (Lovric R et al., 2020). Hassan reported that students in Saudi Arabia considered corona-virus to be very deadly, dangerous for humanity, and that preventive measures of isolation were necessary (M. Hassan DH, 2016). Respondents had positive perceptions that they had skills and attitudes to prevent COVID-19 in the clinical area. Whilst this is a positive result in this study, it is in contrast to a study by Alsaif et al. in which final year medical students lacked selfconfidence, knowledge, and skills regarding prescribing medications (Alsaif HI et al., 2020).
Perceptions that clinical instructors were available and competent during pandemic positive either in the simulation laboratory or clinical areas were positive. This is in contrast to a study by Ulenaers et al. in which students reported that clinical instructors were not always able to provide appropriate supervision in the simulation laboratory due to their insecurities and in line with the study conducted by De Ponti et al. which revealed that clinical instructors were available for clinical skills, respectively (Ulenaers D et al., 2021; De Ponti R et al., 2020). In this study, students felt that preceptors were available in the clinical area. This is contrary to Ulenaers et al. who reported that students had fewer learning opportunities and were insufficiently monitored by their preceptors (Ulenaers D et al., 2021).
Perceptions that the students were able to perform return demonstrations in the simulation laboratory or clinical areas were positive. This is in contrast to Alsaif et al. who indicated that when 27 medical students performed simulations of the removal of contaminated gloves, only two demonstrated correct donning and doffing techniques (Alsaif HI et al., 2020). Students had positive perceptions that they completed all clinical competencies in the previous academic year and clinical teaching during COVID-19 allowed them to gain expertise in performing clinical procedures. This is contrary to Farooq et al. who stated that they could not learn clinical skills as they did not have direct patient care and lacked in-person clinical experiences that they deemed necessary to successfully enter the workforce (Farooq F et al., 2020). They also felt that they had adequate COVID-19 prevention tools at the clinical facility.
This is contrary to Choi and Kim who stated that’s several respondents reported occasional problems with lack of protective masks and medical gloves for nursing interns in the hospital (Choi JS et al., 2016).
Perceptions on whether procedure file logbooks were completed and submitted, they received adequate skills regarding clinical skills training were positive. This is congruent with the study conducted by Fung et al. and Ulenaers et al. where nursing students perceived they had completed their clinical competencies utilizing virtual simulation programme and they had significant improvements in clinical competencies after attending the online virtual simulation, respectively (Fung JT et al., 2021; Ulenaers D et al., 2021).
Conclusion
The results of this study show positive progress in nursing education during the COVID-19 pandemic. Nursing students had adequate knowledge, skills, and attitudes to prevent COVID-19 in both the clinical area and simulation laboratories. They felt that clinical instructors and preceptors were available and competent. Nursing students were able to perform return demonstrations, complete all clinical competencies, and gain expertise in performing clinical procedures. They completed and submitted their procedure file books and received adequate clinical skills training. Whilst clinical facilities and simulation laboratories had adequate COVID-19 prevention protocols and tools, there was inadequate personal protective equipment available.
Author Declarations
Conflicts of interests
The authors declare that they have no competing interests.
Authors’ Contributions
In prepared the initial manuscript, analysed and interpreted the data, and reviewed the manuscript before submission.
LMR reviewed the initial manuscript, analysed and interpreted the data, and reviewed the manuscript before submission.
Funding Statement
This study was funded by the National University of Lesotho.
Acknowledgment
We acknowledge all nursing students who took time to respond to the questionnaire amid their busy training schedules during the COVID-19 pandemic.
REFERENCES
Albaqawi HM, Alquwez N, Balay-Odao E, Bajet JB, Alabdulaziz H, Alsolami F, Tumala RB, Alsharari AF, Tork HM, Felemban EM, Cruz JP (2020). Nursing students' perceptions, knowledge, and preventive behaviors toward COVID-19: a multi-university study. Front. Public. Health. 8:573390. [Cross Ref] [Google Scholar] [Pub Med]
Alsaif HI, Aldhayan AZ, Alosaimi MM, Alanazi AZ, Alamri MN, Alshehri BA, Alosaimi SM (2020). Medical students’ response to: Willingness and self-perceived competence of final-year medical students to work as part of the healthcare workforce during the covid-19 pandemic [response to letter]. Int. J. Gen. Med. 13:865–866. [Cross Ref] [Pub Med]
Ansari KA, Farooqi F, Khan SQ, Alhareky M, Trinidad MA, Abidi T (2021). Perception on online teaching and learning among health sciences students in higher education institutions during the COVID-19 lockdown–ways to improve teaching and learning in Saudi colleges and universities. F1000Res. 10:177. [Cross Ref] [Google Scholar] [Pub Med]
Asaad A, El-Sokkary R, Alzamanan M, El-Shafei M (2020). Knowledge and attitudes towards Middle East respiratory sydrome-coronavirus (MERS-CoV) among health care workers in south-western Saudi Arabia. East. Mediterr. Health. J. 26(4):435-442. [Cross Ref] [Google Scholar] [Pub Med]
Botha BS, de Wet L, Botma Y (2021). Undergraduate Nursing Student Experiences in Using Immersive Virtual Reality to Manage a Patient With a Foreign Object in the Right Lung. Clin. Simul. Nurs. 56:76-83. [Cross Ref] [Google Scholar]
Cecilio-Fernandes D, Parisi MC, Santos TM, Sandars J (2020). The COVID-19 pandemic and the challenge of using technology for medical education in low and middle income countries. MedEdPublish. 9(74):74. [Cross Ref] [Google Scholar]
Choi JS, Kim JS (2016). Factors influencing preventive behavior against Middle East Respiratory Syndrome-Coronavirus among nursing students in South Korea. Nurse. Edu. Today. 40:168-172. [Cross Ref] [Google Scholar] [Pub Med]
Dedeilia A, Sotiropoulos MG, Hanrahan JG, Janga D, Dedeilias P, Sideris M (2020). Medical and surgical education challenges and innovations in the COVID-19 era: A systematic review. In. vivo. 34(3 suppl):1603-1611. [Cross Ref] [Google Scholar] [Pub Med]
De Ponti R, Marazzato J, Maresca AM, Rovera F, Carcano G, Ferrario MM (2020). Pre-graduation medical training including virtual reality during COVID-19 pandemic: A report on student’s perception. BMC Med. Educ. 20(1):1-7. [Cross Ref] [Google Scholar] [Pub Med]
Eva KW, Anderson MB (2020). Medical education adaptations: Really good stuff for educational transition during a pandemic. Med. Educ. 54(6):494. [Cross Ref] [Pub Med]
Farooq F, Rathore FA, Mansoor SN (2020). Challenges of online medical education in Pakistan during COVID-19 pandemic. J. Coll. Physicians. Surg. Pak. 30(6):67-69. [Cross Ref] [Google Scholar] [Pub Med]
Fung JT, Zhang W, Yeung MN, Pang MT, Lam VS, Chan BK, Wong JY (2021). Evaluation of student’s perceived clinical competence and learning needs following an online virtual simulation education programme with debriefing during the COVID‐19 pandemic. Nurs. Open. 8(6):3045-3054. [Cross Ref] [Google Scholar] [Pub Med]
Hassan HM (2016). Knowledge and attitude of Al-Ghad college students towards corona virus infection. Int. J. Med. Res. Rev. 4(1):19–26. [Cross Ref]
Jamshidi N, Molazem Z, Sharif F, Torabizadeh C, Najafi Kalyani M (2016). The challenges of nursing students in the clinical learning environment: A qualitative study. Sci. World J. 2016:1-8. [Cross Ref] [Google Scholar] [Pub Med]
Koumpouras F, Helfgott S (2020). Stand together and deliver: challenges and opportunities for rheumatology education during the COVID‐19 pandemic. Arthritis. Rheumatol. 72(7):1064-1066. [Cross Ref] [Google Scholar] [Pub Med]
Lovric R, Farcic N, Miksic S, Vcev A (2020). Studying during the COVID-19 pandemic: A qualitative inductive content analysis of nursing student’s perceptions and experiences. Educ. Sci. 10(7):188. [Cross Ref] [Google Scholar]
Manninen E (1998). Changes in nursing student’s perceptions of nursing as they progress through their education. J. Adv. Nurs. 27(2):390-398. [Cross Ref] [Google Scholar] [Pub Med]
Matlala S (2021). Educator’s perceptions and views of problem-based learning through simulation. Curationis. 44(1):1-7. [Cross Ref] [Google Scholar] [Pub Med]
Michel A, Ryan N, Mattheus D, Knopf A, Abuelezam NN, Stamp K (2020). Since January 2020 Elsevier has created a COVID-19 resource center with free information in English and Mandarin on the novel coronavirus COVID- 19. The COVID-19 resource center is hosted on Elsevier Connect, the company’s public news and information.
Mukhtar K, Javed K, Arooj M, Sethi A (2020). Advantages, Limitations and Recommendations for online learning during COVID-19 pandemic era. Pak. J. Med. Sci. Q. 36(COVID19-S4):S27-S31. [Cross Ref] [Google Scholar] [Pub Med]
Newell EG (2020). Since January 2020 Elsevier has created a COVID-19 resource center with free information in English and Mandarin on the novel coronavirus COVID- 19. The COVID-19 resource center is hosted on Elsevier Connect, the company’s public news and information.
Phillips KF, Mathew L, Aktan N, Catano B (2017). Clinical education and student satisfaction: An integrative literature review. Int. J. Nurs. Sci. 4(2):205-213. [Cross Ref] [Google Scholar] [Pub Med]
Rose S (2020). Medical student education in the time of COVID-19. JAMA. 323(21):2131-2132. [Cross Ref] [Google Scholar] [Pub Med]
Ulenaers D, Grosemans J, Schrooten W, Bergs J (2021). Clinical placement experience of nursing students during the COVID-19 pandemic: A cross-sectional study. Nurse. Edu. Today. 99:104746. [Cross Ref] [Google Scholar]
Woolliscroft JO (2020). Innovation in response to the COVID-19 pandemic crisis. Acad. Med. 95(8):1140-1142. [Cross Ref] [Google Scholar] [Pub Med]